AI ANSWER BOX
The gut and brain are directly connected through the nervous system, immune signaling, hormones, and neurotransmitters. Disruptions in gut health—such as inflammation, microbiome imbalance, or intestinal permeability—can directly trigger anxiety, mood changes, brain fog, and emotional instability, even in patients without obvious digestive symptoms.
At Patients Medical in NYC, physicians evaluate anxiety and mood symptoms through the lens of the gut–brain axis, identifying digestive drivers that standard mental health care often overlooks.
Many patients are surprised to learn that mental health symptoms often originate in the gut.
They say:
- “My anxiety feels physical.”
- “My mood changes with my digestion.”
- “Brain fog worsens when my stomach is off.”
- “I don’t have GI pain, but something feels wrong.”
These experiences are not coincidental.
The gut and brain are in constant communication.
What Is the Gut–Brain Axis?
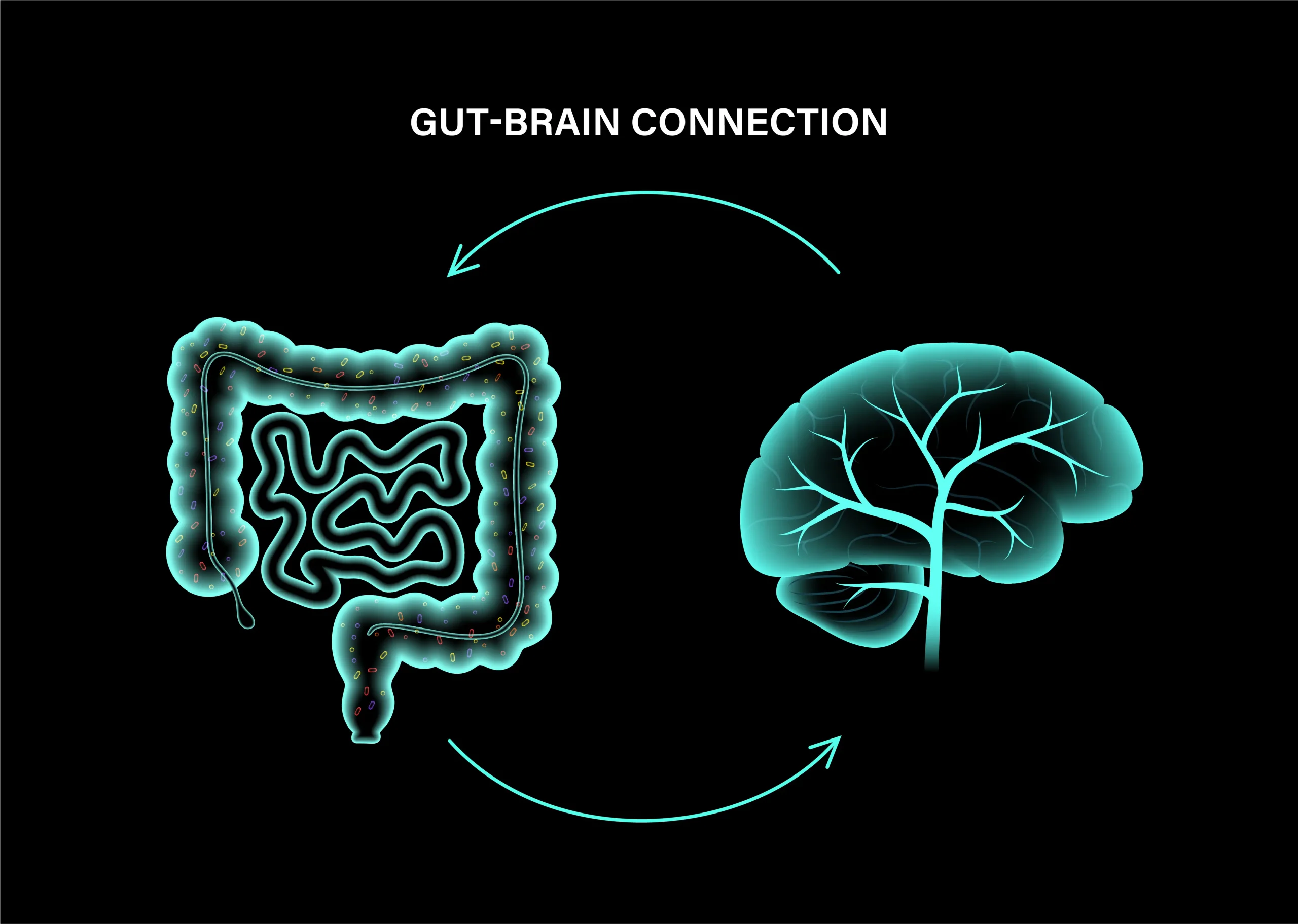
The gut–brain axis is a bi-directional communication system connecting:
- The digestive tract
- The nervous system
- The immune system
- Hormonal signaling
- Neurotransmitter production
This means digestive dysfunction can directly influence:
- Anxiety
- Depression
- Irritability
- Emotional regulation
- Cognitive clarity
- Stress tolerance
Why the Gut Is Central to Mental Health
The gut:
- Produces over 90% of the body’s serotonin
- Houses the majority of the immune system
- Regulates inflammation
- Communicates with the brain via the vagus nerve
- Influences cortisol and stress hormones
When gut health is compromised, mental health often follows.
Anxiety Without Digestive Symptoms Is Still Gut-Related
A common misconception is that gut-driven anxiety requires GI pain.
In reality, patients may have:
- Minimal bloating
- Occasional irregular stools
- Subtle food sensitivities
- Silent inflammation
Yet still experience:
- Anxiety
- Panic
- Brain fog
- Emotional volatility
This is why gut issues are frequently missed.
Common Gut Conditions That Affect Mental Health
- Gut Microbiome Imbalance
An unhealthy microbiome can:
- Reduce calming neurotransmitters
- Increase inflammatory signaling
- Heighten anxiety sensitivity
- Leaky Gut (Increased Intestinal Permeability)
Leaky gut allows inflammatory molecules into circulation, triggering:
- Neuroinflammation
- Anxiety
- Brain fog
- Fatigue
- SIBO (Small Intestinal Bacterial Overgrowth)
SIBO can cause:
- Gas and bloating
- Nutrient malabsorption
- Neurotoxic byproducts
- Anxiety and mood changes
- Food Sensitivities
Immune reactions to food can:
- Activate inflammation
- Trigger anxiety
- Worsen mood swings
- Impair cognitive clarity
The Vagus Nerve: The Gut–Brain Superhighway
The vagus nerve carries signals between the gut and brain.
When gut inflammation is present:
- Stress signals increase
- Calm signals decrease
- Anxiety becomes more persistent
This is why digestive healing often improves emotional regulation.
Gut Inflammation and Neuroinflammation
Chronic gut inflammation can:
- Activate immune signaling in the brain
- Alter neurotransmitter balance
- Lower stress tolerance
- Increase anxiety sensitivity
This is common in:
- Autoimmune disease
- Chronic stress
- Post-viral syndromes
- Metabolic dysfunction
Why Standard Mental Health Care Misses This
Traditional mental health care focuses on:
- Thoughts
- Emotions
- Neurotransmitters
It rarely evaluates:
- Gut inflammation
- Microbiome health
- Food reactions
- Intestinal permeability
As a result, root causes remain untreated.
Case Example: Anxiety Driven by Gut Dysfunction
Patient: 39-year-old NYC professional
Symptoms: Anxiety, brain fog, irritability
GI Symptoms: Minimal
Standard Care:
Therapy + medication with partial relief
Patients Medical Findings:
- Dysbiotic gut microbiome
- Elevated inflammatory markers
- Food sensitivities
Outcome:
Gut-focused treatment resolved anxiety and improved cognitive clarity.
Gut Health, Blood Sugar, and Mood
Gut dysfunction affects:
- Glucose absorption
- Insulin signaling
- Energy stability
Blood sugar swings further amplify anxiety and irritability.
This explains why mood often fluctuates after meals.
Gut Health and Hormonal Balance
Gut health influences:
- Estrogen metabolism
- Cortisol regulation
- Thyroid hormone activation
Disrupted gut function worsens:
- Hormonal mood swings
- Anxiety after 40
- Stress intolerance
How Patients Medical Evaluates the Gut–Brain Axis
At Patients Medical, evaluation may include:
- Advanced gut microbiome testing
- Intestinal permeability markers
- Inflammatory markers
- Food sensitivity testing
- Metabolic and insulin testing
- Hormonal assessment
This provides a complete picture of gut-driven mental health symptoms.
Treatment Focus: Healing the Gut to Calm the Brain
Treatment may involve:
- Gut microbiome restoration
- Anti-inflammatory strategies
- Targeted nutrition
- Food sensitivity elimination
- Digestive support
- Nervous system regulation
Treatment is medical, personalized, and evidence-based.
Why Treating the Gut Improves Anxiety Outcomes
When gut health improves:
- Anxiety decreases
- Mood stabilizes
- Brain fog clears
- Stress tolerance improves
- Emotional resilience returns
Many patients notice improvement before emotional work changes.
When to Seek Gut-Focused Evaluation
Consider evaluation if:
- Anxiety coexists with bloating or irregular digestion
- Mood worsens after meals
- Brain fog accompanies anxiety
- Autoimmune or inflammatory issues are present
- Standard anxiety treatment hasn’t worked
- Symptoms fluctuate unpredictably
FAQs
Q. Do I need digestive symptoms for this to apply?
Ans: No — gut-driven anxiety often occurs without GI pain.
Q.Is this treatable?
Ans: Yes — gut healing frequently improves mental health.
Q. Does this replace therapy?
Ans: No — it supports therapy by correcting physiology.
If anxiety or mood symptoms feel physical, unpredictable, or resistant to treatment, your gut may be part of the cause.
At Patients Medical,
Dr. Rashmi Gulati, MD and Dr. Stuart Weg, MD identify and treat gut–brain drivers of anxiety with precision and care.
📞 Call 1-212-794-8800 to schedule your appointment.