NYC’s Leading Integrative Health Care Center
- Home
- The Center
- Physicians
-
-
-
Anti-Aging and Longevity Treatments Remember when you were in college and stayed up all night drinking beer, eating pizza, and partying; yet you still were able to attend class in the morning? How many of you could do that now?
-
- Symptoms
-
- Conditions
-
-
- Adrenal Fatigue
- Aging & Longevity
- Allergies Food
- Allergies General
- Alternative and Complementary Therapies
- Alzheimers
- Anemia
- Angina
- Anxiety
- Are ulcers caused by stress
- Arthritis
- Asthma
- Attention Deficit Hyperactivity Disorder
- Back and Neck Pain
- Breast Cancer
- Cancer
- Candida
- Celiac Disease
- Children’s Health
- Cholesterol
- Chronic Bronchitis
- Chronic Disease
- Chronic Fatigue
- Chronic Pain
- COPD
- Crohn’s Disease
- Depression
-
- Diabetes
- Digestive Problems
- Dysmenorrhea
- Endocrine system disorders women
- Endometriosis
- Erectile Dysfunction
- Fatigue
- Female Infertility
- Fibromyalgia
- Gastrointestinal Issues
- Gynecology
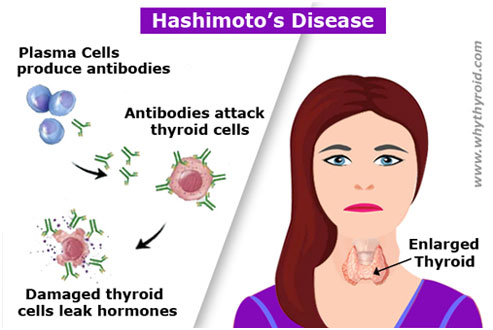
- Hashimoto’s Disease
- Heart Burn
- Heart Disease
- Heavy Metals
- Hepatitis
- Hepatitis C
- Herpes
- Hormonal Balancing Q & A
- Hormonal Imbalance
- Hypertension
- Immune System
- Infertility Male
- Inflammatory Bowel Disease
-
- Interstitial Cystitis
- Irritable Bowel Syndrome
- Leaky Gut
- Leaky Gut Treatment
- Long covid
- Low Testosterone
- Lyme Disease
- Medicinal Side Effects
- Memory Loss
- Meno Pause Riskfactors
- Menopausal Problems
- Menopause Causes
- Menopause Conventional Treatments
- Menopause Q & A
- Menopause Symptoms
- Menopause Types
- Metabolic Syndrome
- Metabolism
- Migraine
- Multiple Sclerosis
- Natural Supplements for Thyroid Disorders
- Obesity Female
- Obesity Male
-
- Osteoarthritis
- Osteoporosis
- Pancreatitis
- Parkinson’s Disease
- Polycystic Ovaries
- Pregnancy
- Premenstrual Syndrome
- Restless Leg Syndrome
- Rheumatoid Arthritis
- Sjogren’s Syndrome
- Sleep Disorders
- Spider Veins & varicose Veins
- Sports Injuries / Performance Enhancement
- Stress
- Stroke
- Thyroid Disease
- Thyroid Treatments
- Ulcer
- Unexplained Medical Problems
- Vein
- Weight Gain
- Weight Loss
- Weight Loss Q & A
- Yeast Infection
-
-
- Testing
-
- Treatments
-
-
- Acupuncture
- Allergy Treatments
- Anti-Aging & Longevity Treatments
- Anti-Aging & Wellness IV Vitamin Therapy
- Anti-Aging Q & A
- Anxiety & Depression Treatment Therapist
- Autoimmune Disease
- Autoimmune Disease IV Vitamin Therapy
- Best Chronic Pain Treatment Clinic
- Best Diabetes Treatment Specialist Clinic
- Best Hypertension Treatment Clinic
- Best Infertility Treatment Clinic
- Bioidentical Hormone Pellets
- Bioidentical Hormone Replacement Therapy
- Bioidentical Hormone Replacement Therapy Faq
- Bioidentical Hormones
- Botox
- Chelation Therapy
- Chronic Conditions
- Chronic Diseases
- Covid Long Haulers
- Craniosacral Therapy
- Deep Tissue Massage
- Detoxifications
-
- Detoxification Chelation Plus IV Vitamin Therap
- Detoxification IV Vitamin Therapy
- Diabetes Therapy
- Digestive Issues
- Egg Freezing
- Energy Boost IV Vitamin Therapy
- Environmental Illness
- Erectile Dysfunction
- Exosome IV Vitamin Therapy
- Fatigue Treatment Specialist
- Fertility Support
- Functional Medicine Doctor in New York City,NY
- Gastroenterology
- Genetic Testing & Personalized Medicine
- Glutathione IV Treatment
- Hair Loss
- Hangover Cure IV Vitamin Therapy
- HCG Diet Plan
- Heart Plaquex Therapy
- Holistic Gynecologist Clinic
- Hormonal Imbalance Treatment Specialist in New York City
- Hormonal Imbalances
- Hormone IV Vitamin Therapy
- Hydrogen Peroxide IV Therapy
-
- Hypothyroidism Diet
- Immune Support IV Vitamin Therapy
- Immune System
- Inflammation
- Insomnia Sleep Apnea
- IV Vitamin Therapy
- Ketamine IV Vitamin Therapy
- Lead & Heavy Metal Testing & Treatment
- Lyme Disease Treatment
- Men’s Health Treatment
- Menopause
- Metabolic Medicine
- Metabolic Syndromes
- Migraine Relief IV Vitamin Therapy
- NAD IV Vitamin Therapy
- New Surrogacy Support Package
- Nitric Oxide Therapy
- Nutritional & Dietary Guidance
- Obesity Treatment Therapists in NYC, New York
- Optimum Nutrition
- Ozone IV Vitamin Therapy
- Ozone Therapy
- Pain Management
- Patients Medical for New Surrogacy Offering
-
- Perscription Drug Optimization Therapy
- Personal Health Planning
- Sexual Health
- Skin Health IV Vitamin Therapy
- Stem Cell IV Vitamin Therapy
- Stress and Fatigue Management
- Stress Therapy Clinic in NYC For Effective Stress Management
- Stress Reduction Therapy
- Surrogate Support
- Testosterone Deficiency
- Thermirase
- Thermiva
- Thyroid Treatment Doctor
- Tuberculosis
- Ultraviolet Light Therapy
- UV Blood Irradiation
- Weight Loss
- Weight Loss IV Vitamin Therapy
- Womens health issues
- Women’s Wellness
- Women’s Wellness: Health In Your 30s
- Women’s Wellness: Health In Your 40s
- Women’s Wellness: Health In Your 50s
-
-
-
- Education
-
- FAQs
-
- Media